
How can a problem in the gut impact psychological functioning? What is the gut-brain connection and which areas of psychological functioning are most affected by celiac disease?
Research shows that untreated celiac disease can impact emotions, cognitive ability, behaviors, and more. Anxiety, depression and fatigue are common issues reported in celiac disease patients prior to diagnosis. Side effects of celiac disease can affect the brain in various ways, leading to a lower quality of life for those suffering from untreated celiac disease, and sometimes even after diagnosis, too.
The gut and brain are intimately connected. Just thinking about food can cause the stomach to release fluids and prepare to eat. Some people make decisions based on a “gut feeling,” or experience “butterflies in their stomach” when they are excited or nervous. Others may experience diarrhea whenever they are particularly anxious (called “anxiety poops” or “stress poops” colloquially). These are all examples of how things that happen in the gut can affect the mind and vice versa. So it makes sense that when the gut is suffering because of celiac disease, the mind might suffer, too.
The exact reasons why those with celiac disease can experience negative psychological symptoms are varied, but include:
Some studies reveal complete remission of depression, anxiety and irritability with gluten-free diet, especially with younger populations. Other studies, especially on depression, are associated with mixed results.
Here are a few things you can do after your diagnosis to help your brain recover:
Let’s dive into that last bullet point. Did you know that the way we think creates neural connections in our brains? Humans develop habitual ways of thinking about situations and interpreting the world—they get used to using certain neural pathways. If you’re continually grumpy or sad for years, it becomes easier to feel grumpy or sad rather than happy. It make take effort to seek out and enjoy happiness.
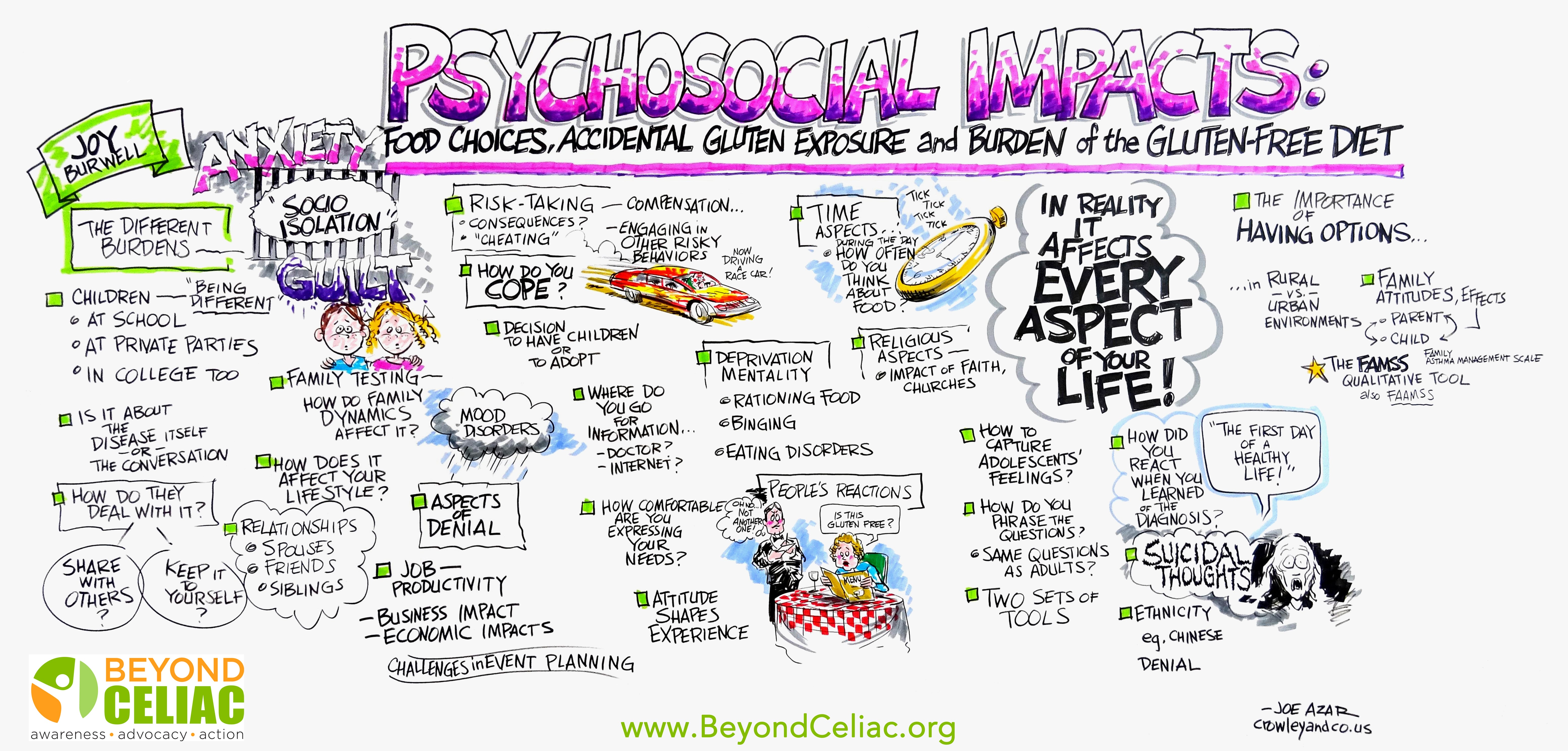
After many years of living in a bubble of discomfort, many forget to really live moments of well-being, satisfaction or joy. An official diagnosis can bring relief to many; however, others can feel emotionally secluded, socially isolated, or anxious and frustrated because of the gluten-free diet.
Some people reconnect with well-being through mindfulness exercises where they learn to “inhabit” happy and peaceful. Soaking up the good vibes, if you will. Meditation has also been found to increase cortical thickness.
Finally, studies show that connecting with others also enhances people’s ability to handle the gluten-free diet. Support groups and online forums can allow you to meet others who have experienced or are experiencing the same things, and counseling or therapy can provide personalized education around coping mechanisms for feelings of isolation and anxiety.
Some possible reasons for continued celiac disease-related mental health problems after starting the gluten-free diet:
It’s important to note that while many people see most of their ailments clear up after starting the gluten-free diet, there are also those that simply have a pre-existing psychological condition, not caused by or related to celiac disease. The gluten-free diet will not affect pre-existing conditions.
Treatments for pre-existing conditions include lifestyle changes and medications. If you take medication regularly, review the ingredients to ensure it is gluten-free. You should avoid medications with wheat starch when possible.
Opt-in to stay up-to-date on the latest news.
Yes, I want to advance research No, I'd prefer not to