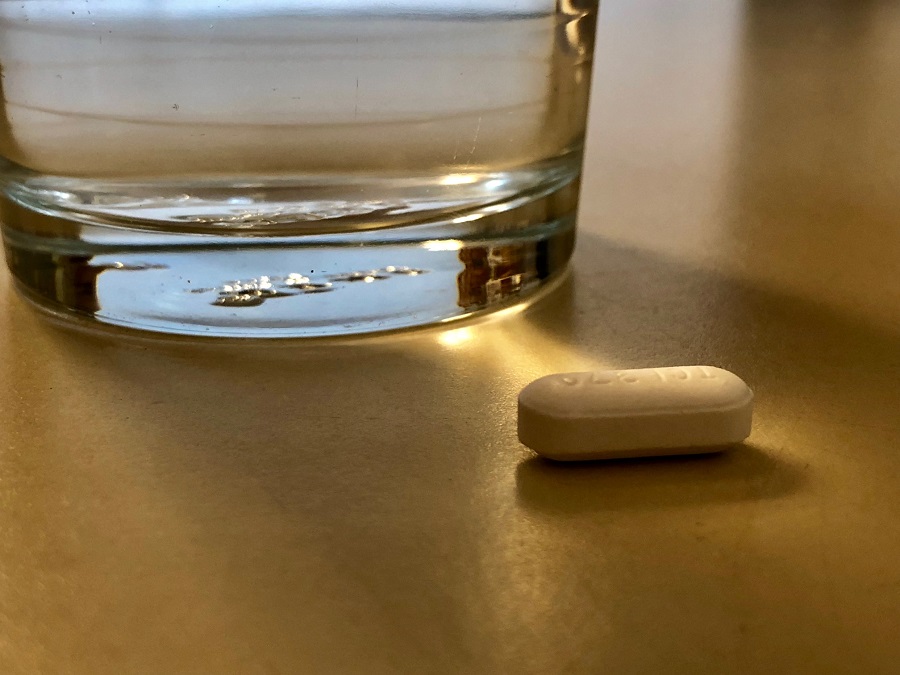
Pill could make small amounts of gluten tolerable and lighten the burden of the gluten-free diet
By Amy Ratner, Medical and Science News Analyst
ZED 1227 sounds like it could be the name of a robot in a future Star Wars movie. But it’s actually a new drug being developed to treat celiac disease.
The drug would work by blocking an enzyme that reacts with fragments of gluten and makes them more recognizable to the cells that cause destruction of the nutrient-absorbing villi in those who have celiac disease.
Phase 2 study begins
The enzyme, tissue transglutaminase (tTG), makes the harmful gluten protein that passes through the intestinal lining more palatable and more recognizable to T-cells. TTG has a direct role in the gut lining where it enhances the inflammatory activity of gluten. By blocking tTG, ZED 1227 would prevent the immune response that drives celiac disease.
![]() Villi: Finger-like projections in the small intestine that help absorb nutrients
Villi: Finger-like projections in the small intestine that help absorb nutrients
![]() T-Cells:
T-Cells:
White blood cells that function as the body’s disease fighting soldiers and are improperly activated by gluten in those who have celiac disease
“You can compare [gluten] to a dangerous bug. In celiac disease, the intestinal immune system does not recognize gluten as a harmless food, which it normally is, but as a dangerous bug, and the tTG makes it worse by causing a better fit of the bug to the immune system,” said Detlef Schuppan, M.D., a celiac disease expert investigating ZED 1227 and director of the Institute of Translational Immunology and Celiac and Small Intestinal Diseases at the University of Mainz in Germany.
Research into ZED 1227 recently advanced to a Phase 2 clinical study, which will test how well the pill works and at what dose. Study participants must have celiac disease and have been on the gluten-free diet for at least one year. They must be generally healthy and have initial biopsies that show no damage.
During the six-week study, patients will eat a cookie containing 3 grams of gluten daily, but otherwise maintain their normal gluten-free diet.
Participants will receive either 10 milligrams (mg), 50 mg or 200 mg of ZED 1227 or a placebo. The results of biopsies done at the beginning of the study will be compared to those done at the end. The primary endpoint, the way in which the success of a study is evaluated, will be how much damage to the intestine, if any, is shown on the biopsies. Patients will also report their symptoms and other factors, called patient reported outcomes, which will serve as a secondary endpoint.
“We want to see what happens if we give increasing doses of the pill, and if we can significantly reduce or even abolish any inflammatory damage to the mucosa,” explained Schuppan. He designed the celiac disease research study along with Markku Maki, M.D., of the University of Tampere, Finland, Knut Lundin, M.D., of the University of Oslo, and Dr. Falk Pharma, a company that specializes in the development of drugs used in gastroenterology. Zedira, a clinical-stage bio-tech company with a focus on celiac disease and transglutaminase, is also involved in development of the drug.
The study is being conducted at 16 medical centers in Europe, including in Germany, Finland, Norway and Ireland. Schuppan said 3 grams of gluten over six weeks should be enough to cause measurable changes in the intestine but not enough to harm study participants. And the expectation is that the gluten would be neutralized by the drug for patients who receive it.
Lightening patients’ load
“Pre-clinical data clearly indicated the pill is able to inhibit the enzyme very significantly,” Schuppan said, noting that in the phase 2 study the range of doses is likely to give researchers a good idea of which works most effectively. “In a way, without tTG, the gluten peptide, even in celiac disease patients, would be relatively harmless.”
Researchers around the world are looking at various ways to treat celiac disease, initially along with the gluten-free diet. The diet is currently the only way to manage the disease, which can cause a wide range of symptoms along with internal damage to the intestine.
Proposed treatments also include: using an enzyme to break down the gluten itself, Interrupting the effects of gluten on the cells lining the intestine, and preventing or interrupting the immune reaction caused by gluten.
Schuppan said that while ZED 1227 is unlikely to eliminate the need for the gluten-free diet, it could significantly improve the lives of celiac disease patients.
“It would take the biggest load from patients shoulders if it could neutralize even a gram of gluten in the daily diet because they would not have to live as restricted as they now are,” he said. He noted that patients could eat in a restaurant free of worry about gluten from cross-contact. They would also have to be a little less diligent about packaged products that might contain a tiny trace of gluten.
Schuppan said there are a few ways the drug could be used by celiac disease patients, including regularly by patients with refractory celiac disease type 1 and as a medication that patients would take as needed when they want protection from gluten exposure when they eat away from home.
![]() Refractory celiac disease type 1: Celiac disease is marked by a lack of response to a strict gluten-free diet after six to 12 months, with symptoms, intestinal damage and an abnormal population of white blood cells in the gut. Type 1 is the less severe form of the condition.
Refractory celiac disease type 1: Celiac disease is marked by a lack of response to a strict gluten-free diet after six to 12 months, with symptoms, intestinal damage and an abnormal population of white blood cells in the gut. Type 1 is the less severe form of the condition.
Researchers are continuing to recruit study volunteers. They expect to have final results in about 18 months. If results are positive, the drug could move to a phase 3 study investigating how it works over a longer term or with a different level of gluten exposure or in patients who do have symptoms or damage to the intestine.
Currently, there are several drugs in phase 2 study, and only one, Innovate Biopharmaceutical’s larazotide acetate, in phase 3. Experts predict it will take at least five years for any of the drugs to become available to celiac disease patients.
Opt-in to stay up-to-date on the latest news.
Yes, I want to advance research No, I'd prefer not to