New study suggests gluten could be prevented from triggering the damaging immune reaction
By Amy Ratner, Medical and Science Research News Analyst
A potential treatment for celiac disease in which nanoparticles act like a Trojan horse and carry a hidden component of gluten to reprogram the immune system not to react has shown positive early results in a new clinical trial.
In a small Phase 2a study preliminarily presented at a European gastroenterology conference, researchers from Cour Pharmaceuticals outlined how the treatment could potentially prevent gluten from triggering the immune reaction in celiac disease.
Study participants who were given the nanoparticles were able to eat gluten with a substantial reduction in inflammation, according to a press release from Northwestern University, where the research was started in a laboratory run by Stephen Miller, PhD, director of the Interdepartmental Immunobiology Center and a member of the Beyond Celiac scientific advisory council. The results also show “a trend toward protecting patients’ small intestine from gluten exposure.”
| RELATED: Nanoparticles discussed at Beyond Celiac research symposium |
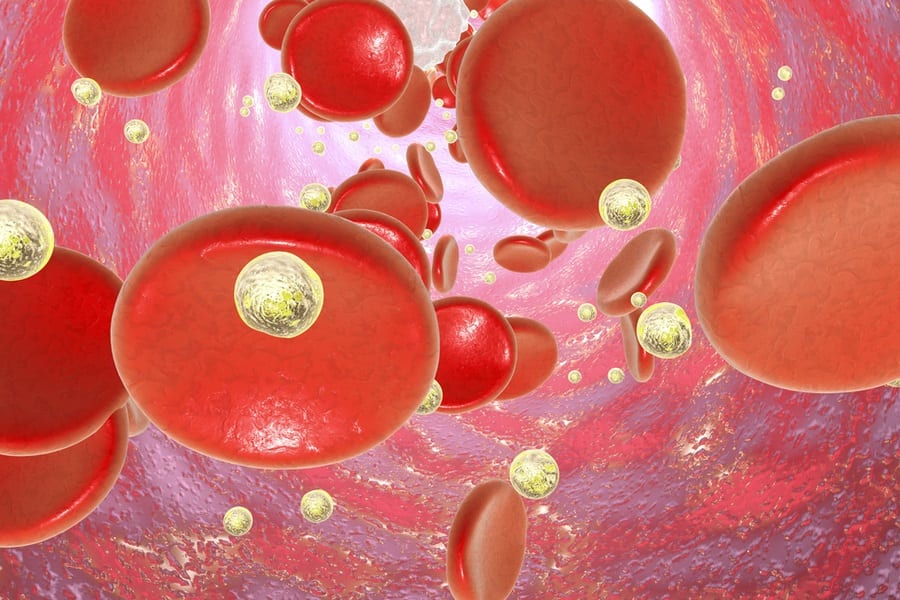
Called CNP-101/Tak-101, the biodegradable nanoparticles form a “friendly shell” containing the fragments of the gliadin portion of gluten. When the nanoparticle is injected into the bloodstream, the immune system does not respond because it sees the particle as “innocuous debris.” The nanoparticle and its hidden cargo are then consumed by a kind of vacuum-cleaner cell in the body.
“The vacuum-cleaner cell presents the allergen or antigen to the immune system in a way that says, ‘No worries, this belongs here,” Miller, a Cour scientific partner, explained. “The immune system then shuts down its attack on the allergen, and the immune system is reset to normal.”
In the clinical trial, 34 patients with biopsy proven celiac disease were given either CNP-101 or a placebo by intravenous infusion (IV) twice over eight days. A week after the second dose, they ate 12 grams of gluten each day for three days, followed by 6 grams of gluten each day for 11 days. A slice of white bread contains about 2 grams of gluten.
Six participants, three each from the treatment and placebo group, did not complete the gluten challenge due to gluten-related symptoms. Study participants who got the medication reported more nausea, headache, abdominal pain and back pain than the placebo group, side effects thought to be related to the IV infusion, though additional studies are needed. The side effects were mild and did not last long, according to researchers.
Those who were given CNP-101 showed 90 percent less immune inflammation than those in the placebo group. Those given the placebo had marked damage to the intestine revealed through biopsies done in all study participants at the start and end of the gluten challenge.
The effect of the nanoparticle treatment was evaluated by looking at pro-inflammatory cytokine interferon-gamma, which is a way of measuring systemic activation of T-cells by gluten. Study participants who were given the drug had 2.1 interferon-gamma spot forming units compared to 17.57 in the placebo group when tested on the sixth day of the gluten challenge.
| T-Cells: White blood cells that function as the body’s disease fighting soldiers and are improperly activated by gluten in those who have celiac disease. |
The research was a double blind, randomized, proof-of -concept study designed to evaluate the effectiveness and safety of CNP-101. It was done by scientists from Beth Israel Deaconess Medical Center, Harvard Medical School and the Mayo Clinic in addition to those from Cour, Takeda Pharmaceuticals and Northwestern University.
| Randomized double blind study: A clinical trial in which neither the researchers nor the patients know whether they are getting the medication or a placebo. Study participants are put into one group or the other at random. |
The typical clinical proof of concept study has approximately 30 subjects, said John J. Puisis, Cour CEO. Based on an interim analysis, the study achieved statistical significance related to the primary endpoint, the measurement of the interferon-gamma spot forming units, Puisis said. The strength of the data led to a decision to move onto Phase 2b studies, he noted.
| RELATED: The phases of clinical study |
“This is the first demonstration the technology works in patients,” Miller said. His laboratory at Northwestern has been working for three decades to refine similar nanotechnology in multiple sclerosis and type 1 diabetes, both autoimmune conditions like celiac disease. The celiac disease findings set the stage to treat these and other diseases as well as peanut allergy and asthma.
Cour describes the nanoparticle treatment as one that “treats the root cause of autoimmune conditions unlike traditional approaches that seek to minimize symptoms using immune suppression.”
Benjamin Lebwohl, MD, director of clinical research at the Celiac Disease Center at Columbia University, who was not involved in the study, said the results of the research are promising, though not yet conclusive.
“The study showed that this medication caused recipients to mount less of an inflammatory response after eating gluten, as measured by blood testing,” said Lebwohl, who has served as a consultant to Takeda. “It is premature to conclude that this drug will allow for full tolerance, that is, prevent symptoms, antibody production, and intestinal damage after eating gluten.”
But he noted that the “signal being seen in this gluten challenge study” is a path that should be explored further, perhaps testing different dosing strategies and measuring various endpoints.
Based on the celiac disease study results, Takeda will obtain the exclusive global license of CNP-101 from Cour for $420 million in future payments and royalties on sales of any commercialized products resulting from the license, according to a Takeda press release.
“Our collaboration with Cour has shown, for the first time, that it is possible to induce specific immune tolerance to a foreign antigen in autoimmune diseases such as celiac disease,” said Asit Parikh, MD, head of Takeda’s gastroenterology therapeutic unit.
Takeda, an international pharmaceutical company with global headquarters in Japan and US headquarters in Massachusetts, plans to begin a study to determine the dose range of the nanoparticle drug in treating celiac disease. Meanwhile, Cour will continue to work on treatments for a variety of other autoimmune diseases in its drug pipeline.
The recent Phase 2a study is expected to be submitted before the end of the year to a peer-reviewed journal for publication.
You can read more about the study here.
Opt-in to stay up-to-date on the latest news.
Yes, I want to advance research No, I'd prefer not to