A review of health insurance claims shows ongoing symptoms lead to ongoing costs

By Amy Ratner, Medical and Science News Analyst
Celiac disease patients face a significant economic burden from higher healthcare costs, according to a new study that reviewed five years of healthcare insurance claims.
The average per-person, per-year cost of all healthcare for celiac disease patients was 22 percent greater than controls in the year before diagnosis, and 41 percent and 25 percent greater in the first and second years of follow-up, the study by researchers from IBM Watson Health, Takeda Pharmaceuticals and Beth Israel Deaconess Medical Center found.
Higher costs peaked in the first year after diagnosis and remained higher than controls in the second year, the study, published in the American Journal of Gastroenterology, concluded. Outpatient services, including visits to specialists and the use of diagnostic services, were the primary driver of high costs, according to the study.
| “Insurance companies often think of celiac disease as a ‘no cost’ disorder, and that is part of the reason they are skeptical of paying for treatments.” |
“The main message from our study, which is different than prior studies, is that a lot of the ongoing cost of celiac disease relates to ongoing symptoms and celiac disease activity,” said Daniel Leffler, MD, a study author and medical director of clinical science at Takeda. “That’s why we suggest that if we had therapies that could improve disease control, this could result in less overall cost to the healthcare system.”
Leffler noted this is an important message because “insurance companies often think of celiac disease as a ‘no cost’ disorder, and that is part of the reason they are skeptical of paying for treatments.” Previous studies have suggested that there are real costs related to celiac disease, and this study helps hone in on what is driving those costs, Leffler said.
In the year prior to diagnosis, those with celiac disease paid an average of about $4,000 more in all healthcare costs than controls, nearly $16,000 compared to about $12,000. In the first year of follow-up, celiac disease patients paid an average of about $8,000 more than controls and in the second year, about $4,000 more.
“This study illustrates the importance of building more awareness of the burden of celiac disease,” said Salvo Alesci, MD, Beyond Celiac chief scientist and strategy officer. “There is a burden born by patients and a burden on the healthcare system. Both can be reduced by accelerating the development of treatments for celiac disease and then making sure they become widely accessible to patients who need them.”
The study added up healthcare resource utilization and costs of 11,000 celiac disease patients and an equal number of controls matched by age, sex, geographic region, healthcare insurance coverage and a comorbidity score based on various chronic medical conditions. Researchers counted all-cause healthcare costs and costs directly related to celiac disease alone. They reviewed claims for inpatient admissions, emergency department visits, gastroenterologist visits, dietitian visits, endoscopic biopsies, gastroenterology imaging and prescription drugs
More than half the nearly $4,000 increase in total healthcare costs from the year before diagnosis to the first year of follow up came directly from celiac disease related healthcare expenses, according to the study. In the year after diagnosis, increases in hospital admissions and outpatient services drove increased all healthcare costs, according to the study.
“By contrast, several indicators of disease severity, such as the likelihood of an inpatient admission, an emergency room visit or a gastroenterologist visit, were lower among celiac disease patients in [the second year of follow-up] compared with the [first year of follow-up or before diagnosis],” study authors wrote.
But study authors note that the true picture of the economic burden of celiac disease is not captured in healthcare insurance claims because they do not include the cost of gluten-free food, consultation with a dietitian that is paid out of pocket by patients or over-the-counter dietary supplements.
Researchers used claims data from 2009 to 2017 in the IBM MarketScan Research Databases, which contain inpatient, outpatient and outpatient drug costs for about 138 million employees and their dependents covered by health insurance plans and 10.2 million retirees covered by Medicare.
In the year before diagnosis, other autoimmune conditions most commonly found in those with celiac disease were thyroid disease, type 1 diabetes, rheumatoid arthritis and Crohn’s disease, the claims data showed. While rheumatoid arthritis occurred similarly in those with celiac disease and controls, the other autoimmune conditions were more common in celiac disease patients.
In addition to other autoimmune diseases, celiac disease patients most commonly had hypertension, chronic pulmonary disease, asthma, depression, heart disease and anxiety. Hypertension was more common in controls, but anxiety and other heart disease were less common.
Prior to diagnosis, those with celiac disease were less likely than controls to be admitted to the hospital, but they stayed longer when they were. The two groups had similar likelihood of visiting the emergency room or having an appointment with an orthopedist. But celiac disease patients were more likely to visit with a general practitioner, a gastroenterologist, a neurologist or other specialist and to have lab work and radiology service. Use of prescription drugs was similar.
In the first and second year of follow-up, celiac disease patients were more likely to access all categories of healthcare than controls. One year from diagnosis, nearly 11 percent more celiac disease patients were admitted to the hospital or visited a neurologist compared to the year before diagnosis. About 3 percent more saw a gastroenterologist, but about 6 percent less had an emergency room visits. In the second year, healthcare in all categories except neurologist, orthopedist and other specialist visits, decreased.
Over all three periods in the study, those with celiac disease were more likely than controls to have seen a dietitian, had gastroenterology imaging and a blood test for celiac disease. Additionally, they were more likely to have been prescribed an antidepressant, anti-anxiety medications, immunosuppressants, prescribed vitamin supplements, proton pump inhibitors and antacids, or budesonide, the anti-inflammatory drug used to treat Crohn’s disease.
In the year prior to diagnosis, those with celiac disease spent about 65 percent of their total healthcare dollars on outpatient services compared to about 60 percent for controls.
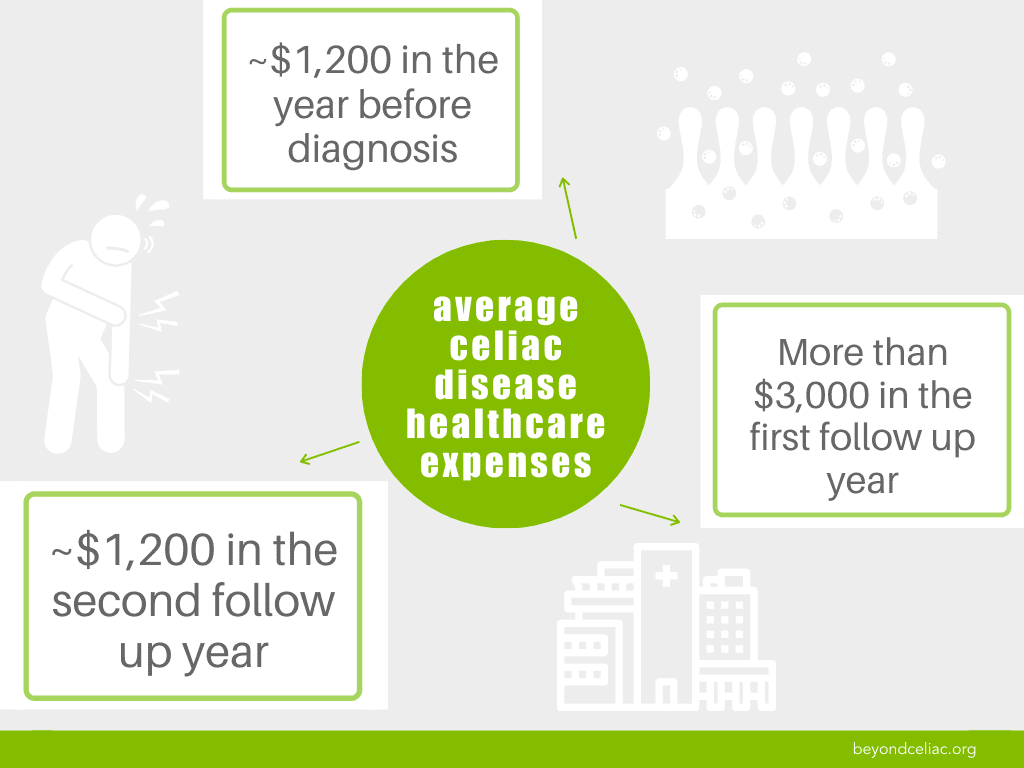
Healthcare expenses directly related to celiac disease averaged $1,200 in the year before diagnosis, more than $3,000 in the year after and returned to about $1,200 in the second follow-up year.
Celiac disease patients used healthcare services related to diagnosis, such as blood testing and gastrointestinal imaging, most often in the year before diagnosis, according to the study. But use of services associated with treatment of complications of celiac disease and accompanying diseases, including other related autoimmune disorders, peaked in the first year of follow-up.
The fact that use of celiac disease related services, including hospital admissions, emergency room visits and specialist visits, remained elevated suggests that they are associated with long-term celiac disease management, the study says. Authors noted that this suggests use of celiac disease related services could be reduced through better options for celiac disease management.
The study faced many of the same limitations typical of studies based on health insurance claims, the authors wrote. These include mistakes or omissions when health claims are coded. Additionally, strict requirements for including celiac disease patients might have excluded those who were diagnosed without a biopsy and some patients with undiagnosed celiac disease might have been included in the control group. Requirements for controls regarding other conditions similar to those of the study participants with celiac disease might have caused the control group to have more healthcare costs and reduced the difference between the two groups.
The study also included only participants who had 36 months of commercial health insurance or Medicare supplemental insurance. “The results may not be applicable to patients who are uninsured, have other insurance or have less stable insurance coverage,” the study says. These patients “may face greater barriers to celiac disease diagnosis and management because they lack access to healthcare providers and services,” the study notes.
At the 2019 Beyond Celiac Research Summit, recognition and understanding of the economic burden of celiac disease by scientists, federal regulators and health insurance companies was identified as key to getting past some of the barriers that have prevented celiac disease research from resulting in new treatment for patients.
Patients, researchers and pharmaceutical company, health insurance and Food and Drug Administration representatives attended the summit. The true economic impact of celiac disease, including missed work and school, as well as use of the healthcare system to deal with both the symptoms and complications of celiac disease is not well understood. Evidence that details these costs could help support the need for new treatments for celiac disease was one of the conclusions of the summit.
You can read more about the study here.
Opt-in to stay up-to-date on the latest news.
Yes, I want to advance research No, I'd prefer not to