What physicians and patients should be on the look out for
By Amy Ratner, Medical and Science News Analyst
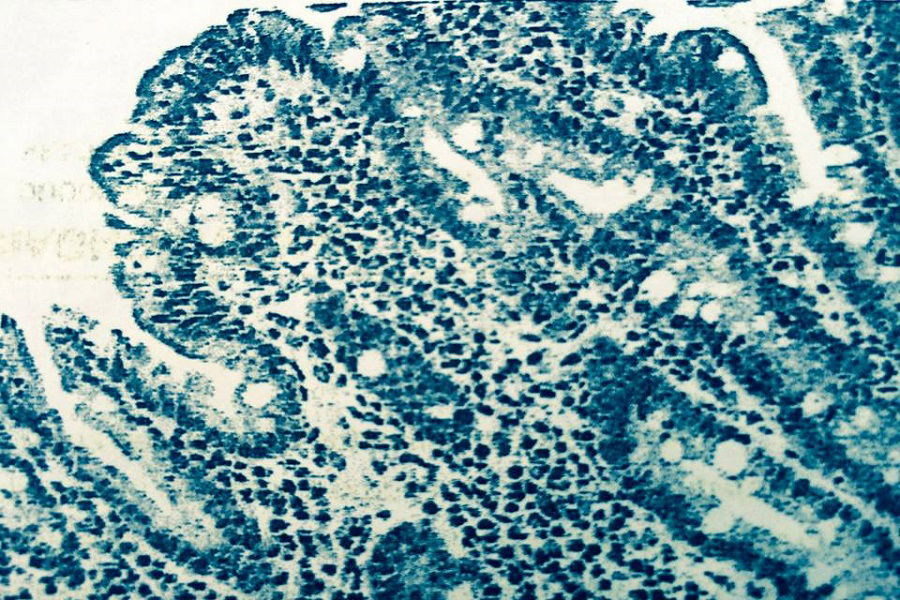
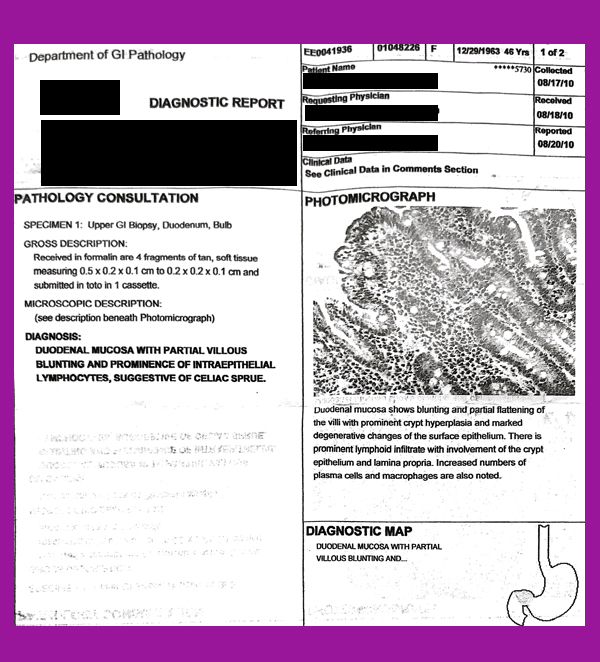
A celiac disease diagnosis should include a biopsy, in which small samples are taken from the intestine and sent to a pathologist for review.
But if you are facing this procedure or have already had it done, it’s possible you didn’t know exactly how the samples are gathered and then interpreted by the healthcare professionals involved in the process.
And you would not be alone. Sometimes even the gastroenterologist who takes the samples, the pathologist who looks at them under a microscope and the doctor who uses the results to make a diagnosis need to be reminded of the steps that result in the best care for patients.
Kendall Egan, of Rye, N.Y., was diagnosed with celiac disease 20 years ago by an internist who told her after an endoscopy and biopsy that the results provided clear evidence she had a malabsorption syndrome.
“I had no idea what they were looking for. I did not know what they did,” Egan said. “I was in recovery when the doctor came in and said you definitely have celiac disease.”
Egan said she had much better understanding of the procedure when she subsequently went to the Celiac Disease Center at Columbia University, where the biopsy was repeated. Her physician explained that he was looking for flattened villi and would take small samples of her intestine. “It was the difference between going to a celiac center versus the gastroenterologist,” Egan said, noting that she hopes things have improved in the years since she had the procedure, particularly when the biopsy is done somewhere other than a celiac center.
A new celiac disease research study in published in the American Journal of Surgical Pathology attempts to improve biopsy diagnosis by describing the best practices in the use of the endoscopy and biopsy for patients with suspected celiac disease. The study lays out workable guidelines that can be used in daily practice.
| Endoscopy: Typically, an outpatient procedure done under sedation and local anesthesia in which a long thin tube with a camera on the end is inserted in the patient’s mouth and makes its way to the small intestine, sending a video image to a monitor allowing the physician to see any obvious abnormalities. Biopsy: The removal of small samples of the lining of the small intestine taken during an endoscopy, which are then studied by a pathologist to determine whether evidence of celiac disease is present. |
Best practices
Marie Robert, M.D., a surgical pathologist at Yale University School of Medicine and chief scientific officer for Beyond Celiac, is the lead author of the study.
She and colleagues conducted a review of the literature addressing endoscopy and biopsy for celiac disease and compiled data to create the best practice recommendations.
The study recommends that:
| Duodenum: The first and shortest part of the small intestine |
| Intraepithelial lymphocytes: White blood cells found in the lining of the small intestine |
“The diagnosis of celiac disease requires close cooperation between clinical, endoscopic and laboratory practices,” the study concludes. Informed dialogue between the specialties is crucial.”
Takeaways for patients
The study is intended to help clinicians and pathologists with the finer points of diagnosis, the authors note. But there are also cealiac disease research takeaways for patients, both before and after the procedure.
“Patients undergoing an upper endoscopic examination in order to consider a diagnosis of celiac disease should verify up front with their gastroenterologist both the number and location of biopsies to be taken,” Robert said. “This is important since the biopsy changes in celiac disease may be patchy and could be missed if the appropriate number of biopsies is not obtained.”
After the endoscopy and biopsy are done, patients should receive a copy of the pathologist’s report.
“The biopsy report should either specify that the biopsy is normal, or, if abnormal, should discuss the villi and presence or absence of inflammation, such as intraepitheial lymphocytes,” Robert explained. “Patients having questions about the pathology report should start by asking their gastroenterologist for clarification. They may also request to speak to the pathologist for more information if questions remain.”
Opt-in to stay up-to-date on the latest news.
Yes, I want to advance research No, I'd prefer not to