Study finds most celiac disease patients have positive tests results for gluten in urine and stool
By Amy Ratner, Medical and Science News Analyst
Celiac disease patients frequently get gluten in their gluten-free diets, according to a recent study that used urine and stool samples to measure real-world gluten exposure.
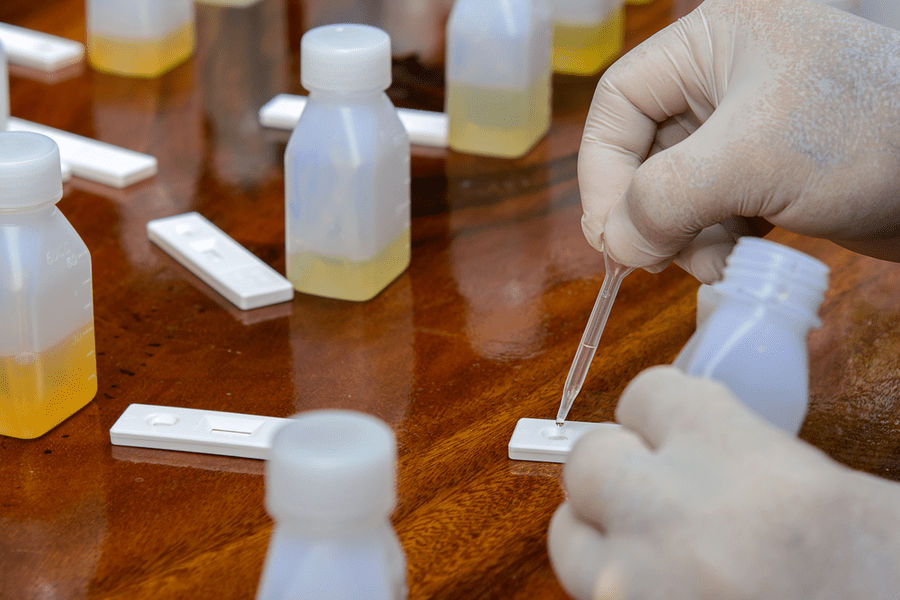
Study participants, all of whom had been on the gluten-free diet for more than two years and considered themselves to be following it strictly, collected stool and urine samples for four weeks. Tests for gluten immunogenic peptides (GIP) were then used to measure how much gluten was in the samples.
| Gluten immunogenic peptides: fragments of gluten proteins that are resistant to gastrointestinal digestion and trigger symptoms and intestinal damage in those who have celiac disease and perhaps symptoms in those who have gluten sensitivity. |
“Most patients in our study excreted GIP at least once during the four week period, which is direct evidence of inadvertent gluten exposure,” wrote authors of the study, which was published in the journal, Clinical Gastroenterology and Hepatology.
| Median: the middle number in an ascending or descending list. In a study, an equal number of the participants are above and below the median. |
The study by researchers from Argentina, Canada and El Salvador found that participants were exposed to gluten a median of three times. Overall, weekend and weekday median gluten exposure was similar, the study says. Stool tests were used to measure gluten at the end of the week and urine tests were used to measure gluten at the end of the weekend.
Study authors note that the tools typically used to determine whether someone is following the gluten-free diet include blood tests, biopsy results, patients’ own reports on adherence and interviews and questionnaires. But they say these measures have “low sensitivity to identify low-level exposure or higher, but occasional exposure. They point to the stool and urine tests as “objective and accurate markers to detect consumption of gluten in the short term.”
Stool tests can detect more than 40 milligrams per day of gluten, while urine tests are positive for 40 to 500 mg per day.
Other studies based on the tests have also concluded that it’s not uncommon for a gluten-free diet to contain gluten even when people with celiac disease are trying hard to avoid it. For example, the DOGGIE bag study led by researchers from Boston Children’s Hospital found that two thirds of patients who were strictly following a gluten-free diet still showed signs of having consumed gluten.
The 53 participants in the new study were recruited from the Celiac Disease Clinic at C. Bonorino Udaondo Gastroenterology Hospital in Argentina. They were put into symptomatic and asymptomatic groups depending on answers to questions about gastrointestinal symptoms on a celiac symptom questionnaire. Study participants were told to follow their normal gluten-free diet.
Nearly 90 percent of all study participants had at least one urine or stool sample that was positive, according to the study. About 94 percent of patients with symptoms had at least one positive sample, while about 86 percent of asymptomatic patients did.
When results of stool and urine sample tests were tallied separately, 62 percent of study participants had at least one positive stool sample, while nearly 70 percent had at least one positive urine sample.
Overall, nearly 38 percent of more than 400 stool and urine samples were positive for GIP, the study found.
Additionally, the number of patients who had samples positive for GIP in both urine and stool increased over the four weeks the study was conducted. The increase could be explained by participants being more “hypervigilant” about their diets at the start of the study, then less so as it progressed, the study says.
Those with symptoms of celiac disease had more weeks in which GIP was detected in stool than patients who had no symptoms.
However, study participants with no symptoms had a significantly higher proportion of evidence of gluten in their urine compared to symptomatic participants. Urine tests measured gluten at the end of the weekend, leading researchers to suggest that patients who don’t have symptoms likely relax their vigilance in the gluten-free diets on the weekends. Also, when patients don’t have symptoms, they lack warning signs that would “prompt them to correct the diet,” the study says.
Objective GIP tests confirm that both those who have symptoms and those who don’t “require strict dietary monitoring,” the authors write, noting that the number of lapses overall is similar for both types of celiac disease patients.
The study looked at connections between urine and stool test results and detection of celiac disease antibodies in blood tests.
The number of samples that were positive for GIP correlated with positive deamidated gluten peptide IgA (DGP) in blood samples, but not with levels of tissue transglutaminase tTG. Symptomatic patients had higher levels of DGP. Study authors note that more investigation regarding connections between GIP and blood test results is needed because there is “controversy regarding the usefulness of DGP antibodies.” TTG testing is widely used to monitor antibodies when celiac disease patients get follow-up care.
“Patients with celiac disease on a long-term gluten-free diet are still frequently exposed to gluten,” the study concludes, noting that tests to detect GIP in stool and urine might be useful in assessing whether a patient is complying with the gluten-free diet.
Lack of biopsy results to determine intestinal damage related to gluten in the diet is a study limitation, according to the authors, who add that biopsies should be considered in future studies. When combined with the results of this study, evidence from biopsies could confirm that continued gluten exposure is most likely the cause of persistent intestinal damage in celiac disease, the study says.
You can read more about the study here.
Opt-in to stay up-to-date on the latest news.
Yes, I want to advance research No, I'd prefer not to